Diabetes is a global health issue affecting millions of people, often impacting daily life, health routines, and long-term wellness. Over recent years, as our understanding of diabetes has evolved, so has our approach to treatment, with promising new options emerging, including stem cell therapy.
What is Diabetes?

Diabetes mellitus, commonly referred to simply as diabetes, is a metabolic disorder where the body either doesn’t produce enough insulin or can’t effectively use the insulin it does produce. Insulin is a hormone that helps regulate blood sugar levels, which is critical to providing cells with the energy they need. When this system is disrupted, blood sugar levels become too high, potentially leading to serious health complications.
Types of Diabetes
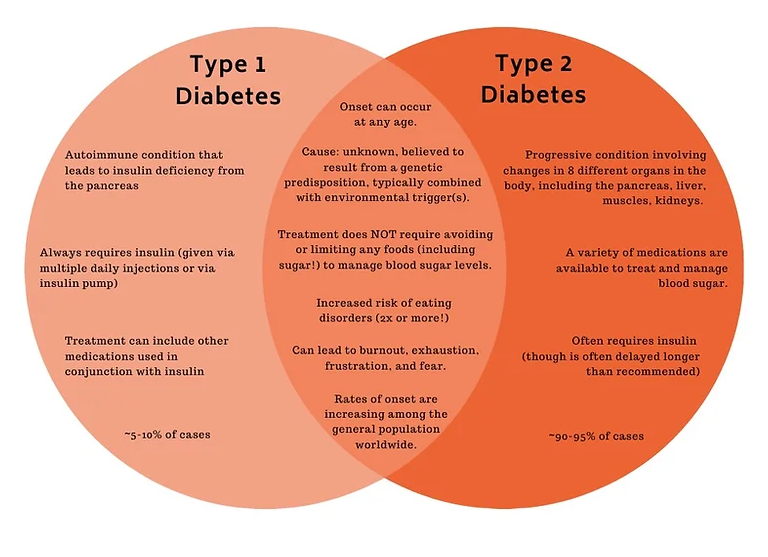
There are three main types of diabetes:
- Type 1 Diabetes: An autoimmune condition where the immune system attacks insulin-producing cells in the pancreas. People with Type 1 diabetes must rely on insulin injections or pumps to regulate their blood sugar levels.
- Type 2 Diabetes: The most common type of diabetes, often associated with lifestyle factors and genetic predisposition. In Type 2 diabetes, the body either doesn’t produce enough insulin or becomes resistant to it.
- Gestational Diabetes: This type occurs during pregnancy when hormone changes affect insulin’s effectiveness. While gestational diabetes typically resolves after childbirth, it can increase the risk of developing Type 2 diabetes later in life.
How Common is Diabetes?
Diabetes is alarmingly common and is on the rise worldwide. The International Diabetes Federation estimates that over 500 million adults globally are living with diabetes, with Type 2 diabetes accounting for over 90% of these cases. This prevalence is driven by lifestyle changes, genetics, and other risk factors.
Symptoms and Causes of Diabetes
Symptoms of Diabetes
The symptoms of diabetes can vary depending on the type and severity but generally include:
- Frequent urination (polyuria)
- Increased thirst (polydipsia)
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Tingling or numbness in the hands or feet (more common in Type 2 diabetes)
These symptoms are often mild in the early stages of diabetes, especially in Type 2 diabetes, which can sometimes delay diagnosis and treatment.
Causes of Diabetes
While the exact causes of diabetes differ depending on the type, several key factors contribute to its development:
- Genetics: A family history of diabetes increases the likelihood of developing the condition.
- Autoimmune Reaction: In Type 1 diabetes, the immune system mistakenly attacks and destroys insulin-producing cells.
- Lifestyle Factors: Poor diet, physical inactivity, and obesity are major contributors to Type 2 diabetes.
- Hormonal Changes: Hormones during pregnancy can make it more challenging for the body to use insulin effectively, leading to gestational diabetes.
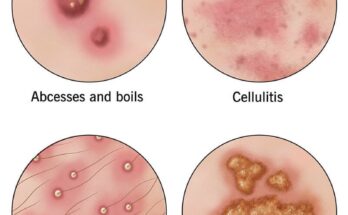
What are the Complications of Diabetes?
If not properly managed, diabetes can lead to a range of severe health complications, including:
- Cardiovascular Disease: Diabetes significantly increases the risk of heart disease, stroke, and high blood pressure.
- Kidney Damage (Diabetic Nephropathy): High blood sugar can damage the kidneys, leading to kidney failure.
- Nerve Damage (Diabetic Neuropathy): Prolonged high blood sugar levels can cause nerve damage, particularly in the legs and feet.
- Eye Damage (Diabetic Retinopathy): Diabetes can damage the blood vessels in the eyes, potentially leading to blindness.
- Foot Damage: Reduced blood flow to the feet increases the risk of infection and complications, sometimes requiring amputation.
Diagnosing Diabetes: Tests and Procedures
Diabetes is diagnosed through a series of blood tests that measure blood glucose levels. Common tests include:
- Fasting Blood Sugar Test: Measures blood sugar levels after fasting overnight.
- A1C Test: Shows average blood sugar levels over the past 2–3 months.
- Oral Glucose Tolerance Test: Measures blood sugar before and after drinking a sugary liquid to assess how the body processes glucose.
If these tests indicate abnormal blood sugar levels, a healthcare provider may diagnose diabetes and begin discussing treatment options.
Stem Cell Therapy: A New Frontier in Diabetes Treatment
Traditional treatments for diabetes include lifestyle changes, medication, and insulin therapy. However, recent advancements in stem cell therapy have opened up promising possibilities for people living with diabetes, especially those who are insulin-dependent.
Stem cells are special cells with the potential to develop into various cell types, and scientists have been exploring their use in treating chronic diseases like diabetes. For diabetes, the goal is to replace or repair damaged insulin-producing cells, allowing the body to better regulate blood sugar levels naturally.
One of the most promising products in this field is Spidex 15, a cutting-edge stem cell therapy designed specifically for managing diabetes.
STEM CELL Product Diabetes Treatment

Spidex 15 is a revolutionary stem cell therapy aimed at helping individuals with diabetes improve their insulin production and regulation. Here’s what makes Spidex 15 a potential game-changer:
- Cell Regeneration: Spidex 15 promotes the regeneration of pancreatic cells that are responsible for producing insulin. By restoring these cells, Spidex 15 may help the body regulate blood sugar more effectively.
- Long-Term Benefits: Unlike temporary insulin injections, Spidex 15 aims to address the underlying issue in diabetes, potentially providing a longer-lasting solution.
- Minimal Side Effects: Traditional diabetes treatments can come with side effects. As a natural approach, Spidex 15 offers an alternative with fewer adverse reactions.
- Improved Quality of Life: By reducing reliance on daily insulin injections, Spidex 15 may make managing diabetes more convenient and less invasive.
How Spidex 15 Works
Spidex 15 uses mesenchymal stem cells (MSCs), which have the unique ability to differentiate into various cell types, including pancreatic beta cells responsible for insulin production. By injecting these stem cells into the body, Spidex 15 works to rebuild damaged cells, supporting a more balanced insulin production system.
The Future of Stem Cell Therapy for Diabetes
While Spidex 15 represents a breakthrough, the field of stem cell therapy for diabetes is still evolving. Research is ongoing to refine and improve treatments, potentially paving the way for even more effective options in the future. As awareness and accessibility of these therapies increase, people with diabetes may soon have new hope for a more manageable and fulfilling life.
Conclusion
Diabetes is a complex, life-altering condition that affects millions. However, with new treatments like Spidex 15, we’re moving closer to more comprehensive and long-lasting solutions. If you or a loved one is managing diabetes, it’s worth exploring the options and understanding the possibilities that stem cell therapy may offer.
What are your thoughts on stem cell therapy for diabetes? Share your perspective or questions in the comments! Let’s continue the conversation on how innovation is transforming the future of diabetes care.